In-Vitro Fertilization
In vitro fertilization (IVF) in the simplest sense is fertilization of a woman’s egg cell outside of her body. It was originally developed as a way to allow women with blocked or absent fallopian tubes to become pregnant.
In vitro fertilization (IVF) in the simplest sense is fertilization of a woman’s egg cell outside of her body. It was originally developed as a way to allow women with blocked or absent fallopian tubes to become pregnant.
This critically timed, carefully coordinated procedure involves removing the mature eggs from a woman’s ovary, fertilizing them with sperm, incubating the resulting embryos in a laboratory under carefully monitored conditions, then transferring the developing embryos into the woman’s uterus with hopes of establishing implantation.
Many patients are surprised to learn that IVF is not their only treatment option. However, IVF would be the first line of treatment for patients with the following conditions:
A healthy egg from a partner or donor
Healthy sperm from a partner or donor
A place for the sperm and egg to meet and grow (a healthy, receptive uterus)
A healthy egg from a partner or donor
Healthy sperm from a partner or donor
A place for the sperm and egg to meet and grow (a healthy, receptive uterus)
We work with sperm banks, egg donors, and agencies to help our patients secure what they need to achieve their parenting dreams. The process can be as simple as ordering donor sperm or locating an appropriate egg donor or gestational carrier, or as complex as planning for all three.
Oral contraceptive pills may begin on day 2 to 4 of your cycle after all pre-treatment testing has been completed. Birth control pills may be taken anywhere from two to five weeks. These will reduce the risk of ovarian cysts forming, aid in the synchronization of follicular growth, and help in the coordination and planning of your fertility care.
An IVF cycle begins with ovarian stimulation and ultrasound monitoring. A baseline pelvic ultrasound will ensure a healthy starting point before initiating medication for the stimulation and assessment of egg production. You will take hormone injections to recruit multiple eggs from your ovaries. During this time, follicular development and hormone levels will be monitored for appropriate growth for several days. Once your follicles have reached the ideal size, you will be ready for egg retrieval.
A custom medication will be administered 36 hours on-site prior to the retrieval of your eggs.
Approximately two to three office visits will be conducted for ultrasounds and for the assessment of blood hormone levels in order to accurately assess egg maturity and in 7-10 days you will be ready for egg collection. Embryon provides daily support onsite for patients uncomfortable self-injecting and for our clients from abroad this support is offered through video calls.
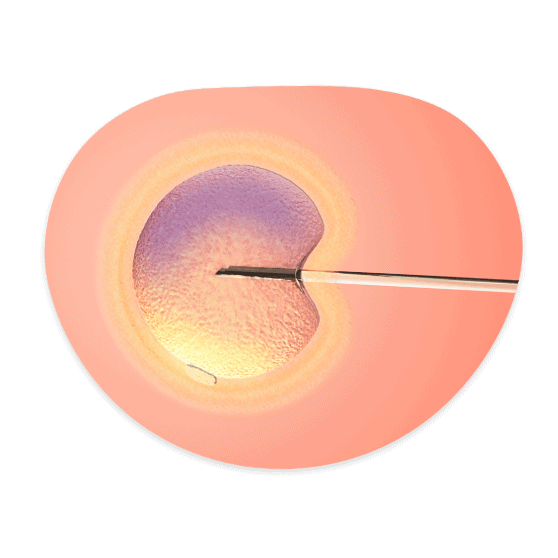
Ultrasound-guided, transvaginal egg retrieval is a procedure in which a long, thin needle is passed through the vaginal wall into the ovary. Our specialist aspirates the follicles from each ovary and the follicular fluid is collected in test tubes, where our embryologist carefully searches for the eggs. The eggs are cleaned, counted, and placed in an incubator. Later that day, the eggs are fertilized with sperm by Intracytoplasmic sperm injection (ICSI) or by traditional IVF.
During IVF, your embryos are cultured between 3 days – 6 days in a temperature-controlled incubator. Each day the embryos are evaluated for quality and development. This information is shared with our specialists to help determine the appropriate day for embryo transfer, which is typically performed on day three or day five of embryo culture. Our embryologists will call you to update you on the embryo quality and to answer any questions you may have.
Embryos are typically transferred back to the uterus on day 3 or day of 5 of their development, when the embryo is at a multicell stage, or day 5 or 6, when the embryo is at a blastocyst stage. This simple procedure usually requires no anesthesia. Your doctor and embryologist will discuss the number of embryos to transfer that will provide you the highest probability of success. You will be given ample time to discuss your embryos and decide on the number of embryos to transfer.
Is a test used to determine the receptivity of the endometrium. ERA may increase the chance of pregnancy by predicting the ideal time for the implantation of the embryo during an IVF cycle.
A biopsy of endometrial tissue is taken and analyzed. Results will indicate whether the endometrium was receptive or non-receptive at the time the biopsy was taken. ERA links to a major improvement of in overall pregnancy rate.
EmbryoGlue is not an actual glue, but acts like glue by increasing the chance of implantation of the embryo to the womb. This transfer medium contains a substance known as hyaluronic acid. Hyaluronic acid is found in the human uterus, and by adding it to the culture media it more closely mimics the natural environment.
Assisted hatching is a scientific IVF technique that requires a laser which creates a hole in the zona of the embryos and in this way it can make it easier for the embryo to “hatch” or breakthrough its outer layer or “shell” by creating an opening. In some situations, this layer is abnormally thick and/or hardened with the freezing and thawing process, among other contributing factors. The less difficulty the embryo has in hatching, the better its chance of attaching or implanting into the wall of the uterus. Pregnancy cannot occur unless the embryo hatches and implants, and assisted hatching can play a key role in realizing these crucial steps.
We will schedule your pregnancy test approximately 10 -15 days after your transfer. When your first pregnancy test is positive, a repeat value will be obtained approximately 48 to 96 hours later. To confirm the positive pregnancy test, we will schedule gestational scan two weeks following the second pregnancy test. At this visit we will be confirming the implantation of embryo(s) and fetal heart motion.
As modern society increases it’s pace, more and more women are postponing starting a family. There can be many reasons which may preclude a woman from starting a family during her most fertile window or selecting to be a mother at a later stage.
Creating a family is a gift at any age and we are here to help. Our team of open-minded experts believes the gift of reproductive medicine should be offered to any patient in need. We have assisted countless women over the age of 50, from Cyprus and beyond, achieve healthy pregnancy without complication. Due to the fact that the uterus ages very slowly, women have the opportunity to create a receptive environment, even at advanced age, for embryos to grow, making the dream of parenthood completely achievable.
A Frozen Embryo Transfer is a cycle in which frozen embryos from a previous IVF or donor egg cycle are thawed and then transferred into a woman’s uterus. A frozen embryo transfer is an option if:
Mini IVF is IVF with a reduced or minimal stimulation protocol. You may see terms like mini, miniature, micro, low stim/stimulation, or even natural to describe this treatment because there is no industry standard terminology. By using less medication , in some cases, one is usually able to produce a small number of high-quality eggs while inflicting less stress on the body and reducing the risk of hyperstimulation. Attributing higher quality to the fewer eggs produced is the motivation for this protocol.
A Natural Cycle IVF involves egg collection aligned with your natural menstrual cycle; there are no stimulation drugs or injections involved. It works in sync with your menstrual cycle to collect the egg naturally selected by your body.

Intrauterine insemination (IUI), also known as artificial insemination, is a fertility procedure in which sperm is washed, concentrated, and inserted directly into a woman’s uterus.
The most common indications for IUI are:
In natural intercourse, only a fraction of the sperm makes it past the woman’s cervical mucus into the uterus. IUI increases the number of sperm in the fallopian tubes, where fertilization takes place.
Studies show that IUI, or artificial insemination, is most successful when it is coupled with fertility drugs that recruit multiple follicles. This technique often is called controlled ovarian stimulation and IUI.
IUI is timed as closely to ovulation as possible, therefore we will medically control the time of ovulation. The insemination is accomplished by placing a speculum in the vagina to visualize the cervix. A catheter containing the sperm will be inserted through the cervical opening into the uterine cavity next to the tubal openings. Depending on which type of treatment is selected, a second sample of sperm is placed in the cervix.
Egg freezing allows a woman to preserve her fertility until she is ready to start her family. Overall, this technology increases a woman’s potential to have children later in life. This option is available to women who are diagnosed with cancer, who require ovarian surgical procedures or experience other illnesses that may affect their fertility.
It is also an option for healthy women who wish to delay attempting to achieve pregnancy until later, knowing that as we age our fertility function decreases. During an egg-freezing cycle, a patient will go through many of the same steps that are involved in a typical IVF cycle: ovulation stimulation, ultrasound monitoring, and egg retrieval. After egg retrieval, the eggs will be cultured for a few hours and then frozen the same day for future use.
Our lab offers 95 % survival rate of oocytes.
An alternative option in fertility preservation is embryo freezing. Once eggs are retrieved, mature eggs are fertilized with either partner or donor sperm. These high quality embryos can remain frozen, if preferred, until the patient is ready to use them. If patients have completed their families, they have the option to donate these frozen embryos to research, anonymously to another couple or discarded.


The importance of a thorough evaluation of both partners in the relationship cannot be overestimated. Male factors account for at least 40% percent of all fertility issues in patients.
Embryo Donation is possible when a surplus of frozen embryo(s) remain after an IVF cycle and are released, anonymously, for the treatment of another person or couple. Most often, the embryos are donated after the woman for whom they were originally created has completed her family.
The donor-conceived child is considered the child of the woman who carries it and her partner, at the time of delivery. The donor male and female partner have no parental rights or responsibilities for a child born following their donation.
The woman receiving the donor embryos and carrying the donor-conceived child is the legal parent. The donor male and female partner have no parental rights or responsibilities for a child born following their donation.
We adhere to the strict screening guidelines for embryo donors.
Embryo Donation is less expensive than Egg Donation and Sperm Donation treatment and a quicker process overall.


Genetic testing is an option we offer that can put patients at ease regarding the health of their embryo(s) in addition to their chances for a successful pregnancy with IVF. Each type of genetic screening is used prior to the embryo transfer procedure in order to help ensure a healthy embryo that is free of abnormalities. These tests identify anomalies in the embryo that might affect implantation, detect serious genetic conditions like Down syndrome and cystic fibrosis.
Our team is here to help guide you and discuss all fertility preservation options for future family building. The most productive step upon first diagnosis is to have an immediate consultation with our fertility specialist to discuss and begin fertility treatments before cancer treatment is even started.
The most successful techniques include obtaining and preserving the female eggs or ovarian tissue or the male sperm or testicular tissue or creating embryos and then freezing them. Your eggs, sperm or embryos will be available for future use when you have completed your cancer treatment and you have been cleared to move forward with achieving pregnancy.
Due to the time sensitivity with cancer treatment, you can expect an expedited treatment plan and to see our specialist for consultation as soon as possible. Our team will work quickly with you and expedite your care so that your cancer treatment is not delayed in any way.

Surrogacy offers hope to prospective parents who face medical and social obstacles to parenthood.
A surrogacy arrangement involves a third-party female carrying a pregnancy for intended parents.
Gestational surrogacy is where the intended mother or an egg donor provides the egg, and the intended father or a sperm donor provides the sperm. The resulting embryo is transferred to the gestational carrier, who then has no genetic connection to the child.
Surrogacy can be a complex and stressful process, but we are experienced in guiding patients through surrogacy, and we have the tools to assist you in navigating this option.
1. Selection
2. Screening
3. Legal Contract
4. Cycle Synchronization
5. Hormonal Therapy
6. Embryo Transfer
7. Pregnancy Success!
Embryon can work with you to utilize a surrogate of your choosing or assist in finding a suitable surrogate. We facilitate the screening process and legal contract process so an IVF cycle can be initiated.
We provide both local and international intended parents many benefits for their surrogacy journey, including:
Embryon Fertility Center is a leading fertility & IVF clinic in Limassol, Cyprus offering world-class fertility treatments for women and couples.
Copyright 2021 © Embryon Fertility Center
All Rights Reserved
Copyright 2021 © embryon
All Rights Reserved
Ovarian and testicular tissue cryopreservation is available for patients who are at risk of losing fertility due to ovarian surgery, cancer or other serious disease or it’s treatment.
Ovarian tissue cryopreservation is the only fertility preserving option available for young girls and for women who need to commence cancer treatment without any delay. This form of fertility preservation is no longer considered experimental for post-pubertal girls and women, and there are now several births reported after the grafting of prepubertal tissue.
